R01 – Redesigning Digital Clinical Decision Support Tool for Implementation of PST for Depression
Principal Investigators
Patrick J. Raue, PhD, Professor, Department of Psychiatry & Behavioral Sciences, University of Washington
Ian M. Bennett, PhD, Professor, Department of Family Medicine and Psychiatry & Behavioral Sciences, University of Washington
Sean Munson, PhD, Professor, Department of Human-Centered Design & Engineering, University of Washington
Project Description
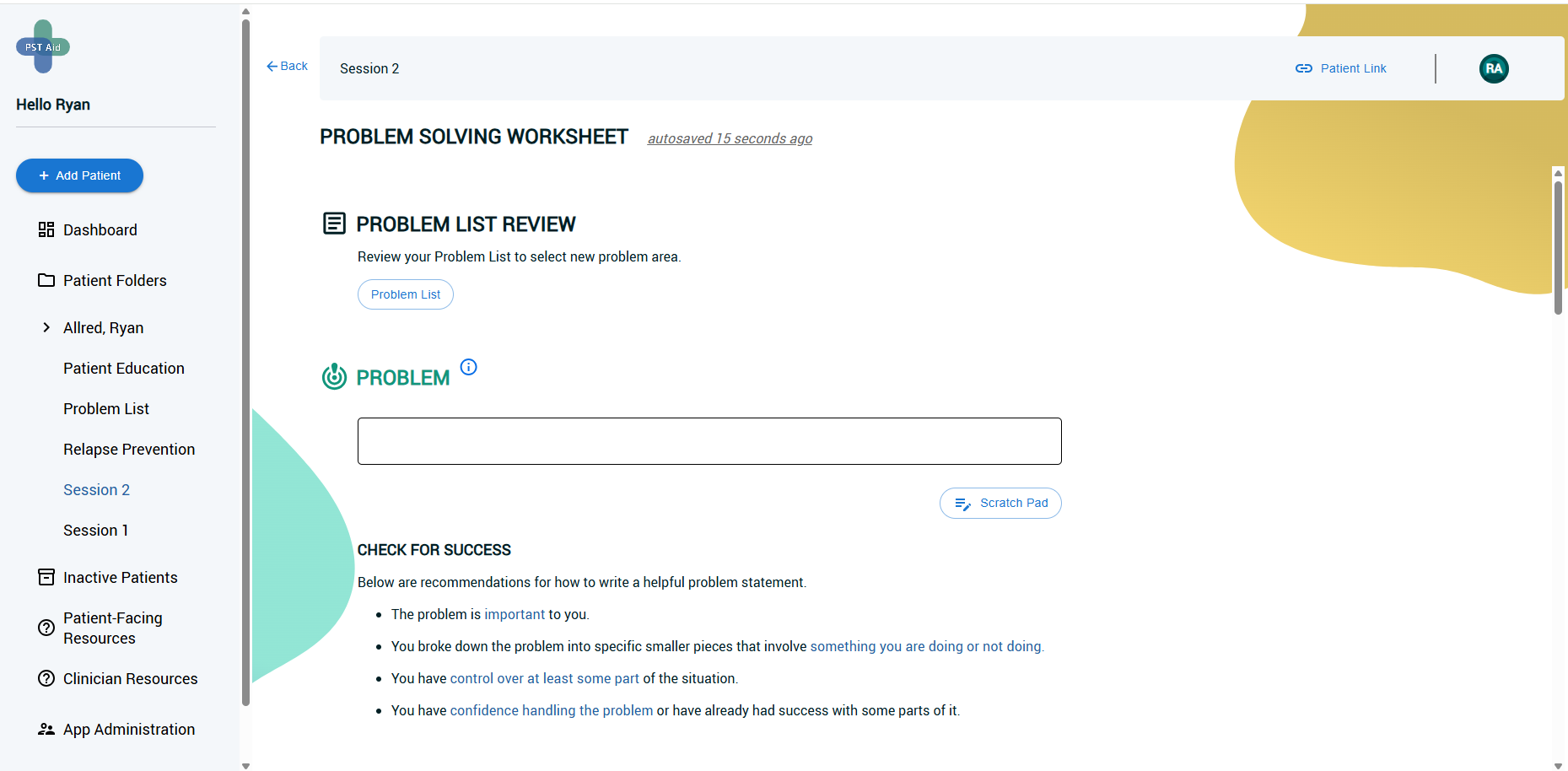
Evidence-based clinical interventions are often delivered with poor fidelity and abandoned by practitioners soon after training. In response to these findings, we have worked with primary care practitioners and patients to co-design an automated decision support tool supporting Problem Solving Treatment (PST) for depression. PST Aid is a web-based app that promotes practitioner–patient collaboration in the use of PST for goal setting and action planning, which we conceptualize as an “educate and reorganize” implementation strategy.
This project started during the first iteration of the UW ALACRITY Center as an R34 project. The current project focuses on redesigning PSTAid by working with clinicians and patients from our partnering OCHIN health informatics network, which includes more than 300 independent community health centers across 45 states serving 130,000 unique patients monthly. We will conduct a hybrid type III effectiveness-implementation randomized clinical trial comparing standard PST implementation with PST implementation augmented by the PSTAid implementation strategy.
| Setting | OCHIN Community Health Centers |
| Population | Adults with depressive symptoms (PHQ-9 > 10), Practitioners |
| Timeline | April 2023 to April 2028 |
Intervention and/or Implementation Strategy Designed or Redesigned
| Intervention | Problem Solving Treatment (PST): an evidence-based, skills-based intervention for depression that teaches patients a 7-step approach |
| Implementation Strategy | PST Aid: a web-based app that promotes provider–patient collaboration in the use of PST for goal setting and action planning |
Anticipated Impact
Patient- and practitioner-centered clinical decision support systems embedded in health information technology tools have the potential to enhance appropriateness, engagement, and usability of PST, an evidence-based practice. The ability to support fidelity to the elements of a clinical intervention, while at the same time reducing burden, would represent a major step forward for the delivery of care and would have implications for a range of other effective, but seldom used interventions. This project will gather invaluable data to inform other clinical interventions that are based in shared decision-making around goals and action plans (e.g., Cognitive Behavioral Therapy, Motivational Interviewing, Behavioral Activation).
Project Publications
Supporting implementation of evidence based psychotherapy through a user centered designed scaffolding technology approach
The Annals of Family Medicine (November 2023) · PDF
Authors
Bennett, I., Mosser, B., Raue, P., Munson, S., & Allred, R.
Abstract
Background: While Problem Solving Treatment (PST) for depression is an effective psychotherapy, it is not widely used and fidelity drops quickly following training. We sought to identify usability challenges and implementation solutions for clinicians who wished to deliver PST and to pilot such a solution.
Methods: As part of the University of Washington ALACRITY Center (NIMH-P50MH115837), we applied the Discover, Design, Build, and Test human-centered design framework. Discover, Design, and Build stages included clinician observations and interviews (9 undergoing PST training-as-usual and 10 experienced PST clinicians), identification of themes and support needs for PST. Rapid prototyping cycles with these clinicians and their patients led to a web-based application which served to support and “scaffold” PST tasks as well as provide decision support for both providers and patients (PST Aid App). Randomization to training in PST as usual or PST-Aid of a new set of providers (clinical social workers who were part of the University of Washington Behavioral Health Integration Program and new to PST) was carried out to pilot a Type III hybrid effectiveness/implementation trial of this tool. Fidelity to PST and clinically significant improvement in depression (PHQ-9 scores) were the outcomes of interest.
Results: 11 clinical social workers were randomized to study conditions (4 PST as usual, 7 PST Aid). No difference was found seen in baseline characteristics of clinicians (p>0.05). Patient age was significantly less in the PST Aid condition than in usual PST (p=0.03) but not for any other demographic characteristic (p>0.05). Baseline depression symptoms scores were not different between study conditions (p=0.43). More clinicians adopted PST in the PST-Aid group than those without the tool (72% vs. 50%; p<0.05). No difference between groups using fisher’s exact test (p = .07) for participants responding to treatment. However, 67% of participants in the treatment arm (PST Aid) responded to treatment, while 0% of participants receiving standard care responded to treatment.
Discussion: We found that a user centered design approach to technology based “scaffolding” can support the adoption, reach, and sustained fidelity of an evidence based clinical intervention. Involving clinicians and patients in the design process may enhance the use and adoption of support tools. This pilot lays the groundwork for a large hybrid effectiveness/implementation trial.